Postpartum depression is more common than you think. 1 in 5 women struggle with postpartum depression (PPD), 1 in 3 women of color struggle with PPD, and 1 in 10 men struggle with it as well. So it is smart if you are researching your risk for postpartum depression.
To help you out, here are some things to think about:
- Family history of depression and anxiety, including PPD
- Personal history of depression or anxiety
- Having multiples
- Inadequate support (family, social, financial)
- ADHD
- Single mothers
- Teen mothers
- Reproductive trauma (infertility, perinatal loss, elected termination, birth trauma)
- Major life transition (moving, new job, deployment)
- Complicated pregnancy
- Difficulty breastfeeding
- Abrupt discontinuation of breastfeeding
- Sensitive to hormone shifts
- History of PMDD (Premenstrual Dysphoric Disorder)
- Endocrine disorders such as Hyper/Hypothyroidism or other reproductive conditions
- Highly sensitive person (HSP)
- Barriers to support, including systemic racism
- Intimate partner violence
- History of sexual, physical, and/or emotional abuse as a child
- Believing the myths of parenthood
- Lack of compassion or inappropriate and unprofessional comments from medical staff before, during, or after delivery
Here are a few more details on some of these risk factors.
Family and Personal History
Family history and personal history of mood and anxiety disorders are something to be aware of. Ask your mom or other female family members what their experience was like giving birth and after. Chances are if you are in your 30s or older, your mom or female family members may not have known due to a lack of awareness, information, or social understanding of PPD. But maybe giving them a chance to share their story might shed some light on whether they would have been screened and diagnosed with PPD if they were to give birth today.
ADHD
ADHD (whether it is treated or not) is also a risk factor. According to a study done in the Netherlands, 57.6 % of women with ADHD are at a higher risk for PPD. One of the many reasons that ADHD can put you at greater risk is that as soon as your baby is born, your estrogen drops drastically.
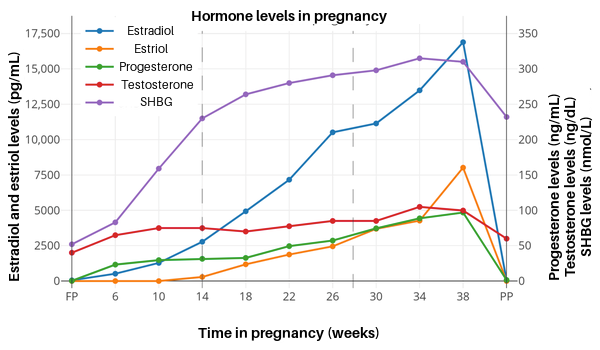
As you can see on the graph, estrogen (estradiol) increases throughout the pregnancy, so some women do experience their ADHD symptoms diminishing during pregnancy.
Estrogen is connected to the neurotransmitters that help manage the executive function system of the brain. People with ADHD have a dysregulation of dopamine and norepinephrine (made from dopamine), so when the estrogen drops dramatically after childbirth, the ADHD symptoms exacerbate.
Reproductive Trauma
You may be wondering what reproductive trauma means. Well, it includes miscarriage (loss up to 20 weeks), stillbirth (loss after 20 weeks), elective termination, infertility, loss of a baby after birth, having a traumatic birth, and post-birth trauma. Families who experience any of these, experience traumatic grief. And traumatic grief can lead to postpartum depression.
Barriers to Support
Barriers to support, specifically for Black, Indigenous, People of Color (BIPOC) is a major reason BIPOC have a higher risk for postpartum depression. BIPOC are not genetically different than others. But they do experience daily chronic stress simply because of their skin color. BIPOC are less likely to seek outside support like therapy due to a warranted distrust of the healthcare system. Plainly put, it is because of systemic racism.
Myths of Parenthood
Common myths of parenthood that contribute to postpartum depression are:
- There is such a thing as a perfect mother/father/parent
- Parents are supposed to self-sacrifice for their children
- Breastfeeding is easy
- If you don’t breastfeed, you aren’t a good mother
- Parenthood is the happiest time in your life
- Postpartum depression is only experienced by a woman who has given birth
- All parents experiencing postpartum depression look depressed
- Depression is the only symptom of postpartum depression (or any perinatal mood and anxiety response)
- The onset of postpartum depression is only a few weeks after delivery
- Parents automatically know what their baby wants and needs by instinct
You are wise to try and figure out whether or not you are at risk for PPD. The more you know, the better your chances are of preventing postpartum depression. Make sure you have a good support system – this is one of the most important resources for prevention. If you are comfortable with also finding a therapist, great, but if not, have people around you that you feel safe talking to about whatever you are experiencing. It will also be important for you to advocate for yourself with your medical team (if you are choosing to give birth at a hospital).
Remember, postpartum depression is common. So if you do experience PPD, that doesn’t mean you are a bad parent, you don’t love your baby, or you won’t get through it. But know that you don’t have to go through it alone.
Jacqueline V. Cohen is a licensed professional counselor and an ADHD-certified clinical specialist provider specializing in perinatal mental health and adult ADHD. To learn more about her services, you can go to her website. You can also contact her by email.
Get your free copy of my e-book: Motherhood and ADHD
You will also receive a subscription to my newsletter.

No comments yet. You should be kind and add one!